AUM researchers use AI to predict antibiotic-resistant UTIs in central Alabama

Researchers at Auburn University at Montgomery (AUM) are using artificial intelligence (AI) to predict antibiotic-resistant urinary tract infections (UTIs) in central Alabama, paving the way for more targeted treatments of one of the most common bacterial infections seen in hospitals and clinics.

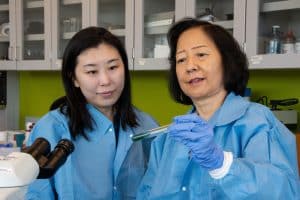
Led by Dr. Li Qian, associate professor of medical and clinical laboratory science, and Dr. Yuan Zhang, assistant professor of management information systems, the interdisciplinary study combines AI with years of clinical data from regional healthcare providers to predict patterns of antibiotic resistance in UTI cases.
The clinical dataset — collected by Dr. Qian in partnership with Baptist Health Medical Center — became the catalyst for the two researchers’ collaboration, enabling them to evaluate and track antibiotic-resistant UTIs in patients across central Alabama.
“Antibiotic resistance isn’t just a global issue, it’s a local one,” Dr. Qian said. “Central Alabama has its own unique microbial landscape, and national guidelines don’t always reflect what’s happening on the ground in local communities.”
Using high-powered computers housed in the College of Business’ Artificial Intelligence Research Laboratory, the team applied machine learning models to analyze the dataset, giving new insights into how clinicians might make more effective, data-driven treatment decisions.
“To our knowledge, this is the first published study using machine learning to address antibiotic-resistant UTIs in patients from central Alabama,” Dr. Zhang said. “By integrating AI into clinical decision-making, we open the door to more personalized and responsive approaches to UTI treatment.”
A growing health challenge

Each year, millions of individuals, especially women, visit hospitals and clinics across the U.S. to be treated for UTIs. Many of these infections, often caused by bacteria such as E. coli, no longer respond to common antibiotics like amoxicillin, Bactrim and nitrofurantoin, leaving patients vulnerable to recurrent UTIs. These recurrent infections can cause serious complications, including kidney and bloodstream infections, sepsis and chronic bladder pain.
“For today’s health care professionals, antibiotic resistance is a growing and critical challenge in treating urinary tract infections,” Dr. Qian said.
Anticipating these challenges, Dr. Qian entered a partnership in 2020 with Baptist Health Medical Center’s Laboratory Services department to collect patient urine samples from its health care facilities and clinics across central Alabama. Tracy Camara, system director of laboratory services for Baptist Health, oversaw the process, which involved gathering cultures from the hospital’s five laboratories. Together, Dr. Qian and Camara built one of the most comprehensive regional datasets of its kind — comprising more than 3,700 urine pathogens. This dataset was crucial to the team’s new study, providing sample sources, pathogen identifications and detailed antibiotic susceptibility results.
“This rich dataset gave us the foundation to develop robust predictive models that reflect the specific health care challenges and patient population in the region,” Dr. Qian said.
Applying AI to Predict Antibiotic Resistance
Armed with this dataset, the researchers began testing AI models capable of evaluating how different antibiotics perform against local bacterial isolates, addressing a pressing need as antibiotic resistance continues to evolve faster than new drugs can be developed.
“In our case, the resistance patterns of E. coli and other organisms isolated in central Alabama did not show higher levels of resistance compared to national or global reports,” Dr. Qian said. “However, by applying machine learning models, we were able to efficiently analyze patterns across large datasets and developed predictive tools tailored to the region’s unique bacterial profile and environment. That level of insight wouldn’t be immediately apparent if a provider were relying solely on national statistics.”
By cleaning the data and ensuring accurate representation of antibiotic outcomes — resistant, intermediate, or sensitive — the team found the study’s dataset responded best to Random Forest and Gradient Boosting, two AI algorithms well suited for analyzing the kind of complex data clinicians encounter in health care settings.
“Our models performed well, achieving about 90% accuracy,” Dr. Zhang said. “That’s a meaningful improvement compared to traditional methods, which often depend on guidelines or lab cultures that take longer to process. Most importantly, we were able to generate insights about antibiotic-resistant UTIs that clinicians can trust and understand.”
The researchers’ early findings show that the type of bacteria in urine samples plays a major role in determining antibiotic effectiveness. Other influential factors included whether the patient was treated as an inpatient or outpatient, along with demographic details influencing resistance patterns.
“These insights not only improved our models but could also guide more targeted treatment decisions in the future,” Dr. Qian said.
While their study was not designed as a public health policy recommendation, its findings point to the importance of localized antimicrobial stewardship.
“With the right data and predictive tools, hospitals and clinics in Central Alabama could make more targeted antibiotic prescribing decisions, potentially reducing overprescribing and slowing resistance,” Dr. Qian said.
Toward smarter, localized care
In March, the team presented their study and findings at the Southern Association for Information Systems Conference, highlighting AI’s potential as a decision-support tool for UTI treatment.
But Dr. Zhang sees broader possibilities for their research.
“Our AI models provide a scalable framework that could eventually be integrated into clinical workflows nationwide,” she said. “The exciting potential here is the ability to offer real-time support to clinicians, giving them evidence-based guidance even before confirmatory lab results are available. The goal isn’t to replace current methods but to enhance decision-making with faster, smarter tools.”

As part of their ongoing research, the team will explore implementing locally informed simulations and testing additional models to improve results. They are also studying whether their AI approach could apply to other infections such as respiratory and wound infections, which also face rising antibiotic resistance.
“We believe machine learning is going to play a much bigger role in infectious disease management,” Dr. Zhang said. “We also expect AI to become more integrated into electronic health records and decision support systems, making them more accessible and user-friendly for clinicians. The aim is not to replace medical expertise but to strengthen it with insights that are faster and more precise.”
In the long term, the team hopes their AI models will be embedded in the decision-support systems used by hospitals such as Baptist Health.
“If implemented thoughtfully, this could help clinicians get real-time resistance predictions at the point of care, supporting faster and more accurate treatment choices,” Dr. Qian said. “Ultimately, the community benefits when health care is safer, faster and more precise. Over time, this data-driven approach could reduce the overall burden of antibiotic resistance in our region, making care more sustainable for everyone.”
